Community Health Workers and Volunteers: The Most Effective Path to UHC
Paid or volunteer?
Community health workers are on the frontlines in many countries—and vital to achieving universal health coverage. Yet the public health community has not reached a consensus on which model is the best.
Consensus is urgently needed, both at the global and country levels, to inform future policies and strategies for strengthening health systems and delivering on UHC.
Based on our experiences in rural Peru and Ethiopia, it’s not either-or. It’s both.
Full-time, paid CHWs form the backbone of family- and community-based services, but there aren’t enough to reach all families. We envision teams of government-paid, full-time CHWs providing comprehensive services to a given population, with a primary health center hub as the base of operations. Each CHW, in turn, would lead a team of part-time community health volunteers providing limited health education and referral services—such as maternal and newborn health, nutrition, hygiene, tuberculosis, malaria, and HIV/AIDS—to a small number of neighboring families.
While paid health workers can do the “heavy lifting” in providing a comprehensive package of services, the volunteers can provide limited, but valuable, preventive and promotional services, such as home visits to vulnerable families or facilitating peer support groups of nursing or pregnant women.
However, these volunteers work most effectively when their geographic and technical scope of work are limited, we’ve learned. A group of volunteers in the jungle of Peru in the 1980s, for example, provided a comprehensive package of services to a large population. In the number of patients seen and the quality of care provided, their services fell short of their paid counterparts. They simply had limited time for training and supervision activities, conducting home visits and meeting regularly with the health team.
In contrast, our experience with volunteers in rural Ethiopia in 1995—providing services to a smaller population—proved quite different. We trained married rural women as CHVs to provide family planning counseling and distribute contraceptives to a limited number of households their own communities. Contraception use increased substantially within a short time, and the majority of CHVs were very satisfied with their workload.
Management Sciences for Health has also followed Ethiopia’s health extension worker program since its inception in the early 2000s. HEWs are full-time, government-paid CHWs, mostly recruited among local women, trained to perform 16 packages of health interventions in their own communities, and they’ve been instrumental in the significant decline of maternal and child mortality. Currently, a majority of Ethiopians receive primary health services from the more than 38,000 HEWs deployed in their communities.
Because HEWs didn’t have enough time to provide widespread preventive and promotional activities, in 2011 the Ethiopian government created cadres of CHVs called women health development armies to provide additional, carefully limited support. The health extension program is working well, but WHDAs are at risk of burnout if they’re asked to take on anything else without incentives.
WHDA volunteers are usually poor, overburdened, and without incentives, a recent evaluation showed. In addition, the government should clearly define how existing primary health centers, CHWs, and volunteers relate to each other to ensure they comprise an effective first link of quality services from replenishment of drugs through patient referrals.
To recruit and retain CHVs, public health programs must understand what motivates them. In Ethiopia and Peru, for example, we learned that while older volunteers can be motivated by the promise of increased social standing, a younger volunteer will see this opportunity to secure a government job or to become a private health practitioner.
Ultimately, CHVs will be considered extraneous to the government health system unless a win-win collaboration can be worked out. Although our efforts in Peru worked within the government’s health structure, we had difficulty convincing authorities to share supplies and drugs to the volunteers. They saw the volunteers as amateurs undeserving of precious resources. Unfortunately, there is little evidence of government health services rewarding increased volunteer performance with a sustainable flow of incentives, training, supervision and supplies.
We will continue to monitor the evolution, successes and limitations of different structures for CHWs. But we see Ethiopia’s HEWs/WHDA model, with its extensive population coverage, embrace of both paid workers and volunteers, and implementation using government structures as a perfect learning ground to roll out widespread primary care—an essential foundation to achieve UHC and the SDGs by 2030.
Luis Tam, MD, DrPH is currently the director of the International Division at Medical Care Development, Inc. (MCDI). From 2014 to 2017, he was the global technical lead for maternal, newborn, and child health at Management Sciences for Health.
Muluken Melese, MD, is senior technical advisor for TB and HIV/AIDS at Management Sciences for Health.
Join the tens of thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday enewsletter, and please share the link with friends and colleagues: http://www.globalhealthnow.org/subscribe.html
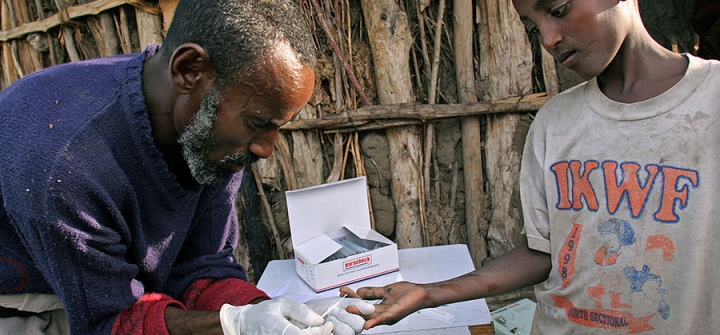
A community health worker in rural Ethiopia tests a boy for malaria. © 2007 Bonnie Gillespie, Courtesy of Photoshare