One Global Health Leader’s Non-Traditional Path
Marian Wentworth’s journey to leading Management Sciences for Health, the global health NGO that works in 36 countries, didn’t have a typical beginning.
Her degree? Mathematics. Her first job after college? Working consultant on operations management for Arthur D. Little, Inc. She followed that up with 27 years at the pharmaceutical giant, Merck. While there, she worked her way up from being a research analyst to leading marketing for the cervical cancer vaccine, Gardasil, and ultimately serving as vice president for Merck’s global vaccines strategy.
In this first of a 2-part Q&A, Wentworth—MSH’s president and CEO since March—shares her thoughts on the pressing need to engage the private sector in global health, the trend towards decentralization, and health systems challenges in low- and middle-income countries.
What do you see as some of the major trends today in global health? Where do you see things going?
One of the things that I see is that new money from donors isn't coming any time soon. Total investment in global health is plateauing and declining depending on what sources you're used to looking at.
That's a mixed blessing. We really have to—as we're looking at global development ideas and initiatives—find ways to deliver value to more than just conventional donors. That might mean when you're talking about health care financing that you bring in private markets and private sector in some way or another. You're learning how to monetize cash out of pocket, et cetera. In any event, I think we have to not only do the right thing but show value to those who are willing to pay for it in one way or another. For me, that's actually also a key to sustainability.
Do you think that the message of delivering value in global health will get traction with the Trump administration?
I think we have traction with Congress. I think we have traction with sectors of the American people. I am not great at playing the game of what's going to happen in politics. I can always hope [but] I guess hope isn't a strategy.
What would you say that most people don't understand about health systems in low and middle income countries?
Let me count the ways. [Laughs.] I think people both miss how much is needed and how much is there. I think it's hard for certain people to envision that a woman who is in her third trimester could easily be a large hike and then a motorcycle ride and then a long truck ride away from a place that has skilled delivery. I think a lot of people actually don't appreciate the logistics of you can really be in the middle of nowhere.
I think on the other side, I think there's a certain belief that … people will do everything the "natural way", which I say in air quotes because it's not safer for a woman to deliver on her own. It's not safer to let diseases just take their course.
For me, getting involved in health system strengthening, I had not been aware of how much actually needs to be done at … the national level in these countries.
One of the things we needed to do in say, the DRC when we start bringing in initiatives to improve supply chain, is we needed to help the MOH actually develop a regulatory framework for approving enough medicine so that you could actually operate under regulatorily approved medicines.
Similarly, in Tanzania we did a program with the [Bill & Melinda Gates Foundation] over I don't know 8 or 10 years of instituting accredited drug sellers. We first needed to come up with an accreditation program and a training program. Then identify money so that these individuals could start their little tiny kiosks. By the time we were done we had thousands and thousands of drug sellers in places that nobody else would be, dispensing antibiotics and contraception and other basic nutrition for infants. Basic things that otherwise these little places would have no health care whatsoever.
Let’s talk about decentralization in health ministries. In Indonesia, for example, the health ministry has undergone a huge decentralization process. What I've heard is this actually makes things much more challenging because at the district level they're getting, “Okay, here are your funds. You decide what to do with them.” Do you see that decentralization is a larger trend in other countries?
Absolutely. I saw decentralization either happening or being talked about in every country that I went to and maybe even the country that I live in.
In Geneva we heard plenty of that. The problem with that is if you've got 50 regions in your country, you've now created essentially 50 different Ministries of Health. Probably 2 of them are going to do a great job and another four of them will do a great job in whatever is of their interest. A bunch of other folks are going to be lost and juggling health care against their other priorities like infrastructure or water or whatever else they're doing.
You're creating, really, an opportunity for worse health care services than you had before. What I have not seen … in the places where I have [been] is that the ministries really have a lot of ability to help regions use these … block grants. As I understand it, decentralization is not all that new. I haven't looked at the trends around decentralization. I'm not surprised it's not new, though, because the politics of it are just universal and enduring.
Right. Let people at the local level decide for themselves.
There's a good argument for closer to the need, closer to the action. The problem is things like health care also require very strong technical skills and getting folks to the point where they universally have the right technical skills to do those things is hard.
Is there a solution to that?
We have to take people where they are. I can spend a lot of time thinking about what forces got them there, but in the end, we go into places where it's hard to work and where we have to roll up our sleeves and figure out how to make it happen. With the decentralization, we've got to ... figure out how we can help build the capacity of that intermediate layer too.
Obviously you know a lot about vaccines from your history at Merck. How do you see where things are headed now in terms of access and development of new vaccines from a global perspective? Are you optimistic in terms of where things are headed?
Yeah. Actually, I am. I think the creation of Gavi was an amazing thing that changed accessibility of vaccines a great deal. They're going through a phase now of trying to figure out what happens with not the poorest of the poor countries as they improve economically and start to graduate out of being in their category of the lowest income nations around the world.
I think one solution to it has been cultivating new manufacturers in parts of the world. I think that has both built more volume for the planet, but also lowered prices for certain key vaccines a great deal. That's in the existing vaccine front. When it comes to new vaccines for various diseases, they're hard. They're really hard. I think Bill Gates himself has publicly expressed his frustration. Vaccines are not easy to develop. They have to be infinitely safe compared to any other kind of medicine. They are not just another medicine. Vaccines go into broader populations of people who are healthy now.
It's got to be right, right, right, right, right before it goes into a little baby. That's a responsibility that many of us take very, very seriously.
Ed. Note: In Part II of this Q&A, Wentworth discusses her leadership style, what it’s like managing a large multinational NGO and advice for students interested in global health.
Wentworth’s Q&A is the first of an occasional GHN series of interviews with global health leaders.
Join the thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday enewsletter, and please share the link with friends and colleagues.
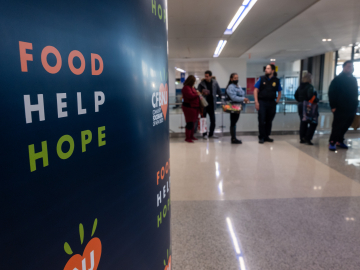
Marian Wentworth confers with health workers at Soroti Regional Referal Hospital in Mbale, Uganda. (Image: Warren Zelman/MSH)