Saving the Future Through the Art of the Knife
“History will judge us by the difference we make in the everyday lives of children,” said Nelson Mandela at the 2002 UN General Assembly Special Session on Children.
1.3 billion children around the world lack access to surgical and anesthesia care.
It’s an appalling gap—not only because so much suffering could be alleviated, but because low- and middle-income countries around the world rely on the younger and future generations for socioeconomic growth.
Children’s surgery is also on the table this week in Davos, Switzerland this week, where the World Economic Forum 2020 is convening 3,000 heads of state, business leaders, policy makers and others to foster public-private cooperation. Wednesday in Davos, the UN Institute for Training and Research launched its Global Surgery Foundation, dedicated to scaling capacity for surgical care in LMICs around the world. And Neema Kaseje, MD, the newly appointed lead of the WHO’s Emergency and Essential Surgical Care Programme and pediatric surgeon, addressed civil society, the private sector, and governments—urging all to do more to ensure children’s access. It is now up to them to walk the walk.
They should keep in mind that children make up almost a quarter of the world’s population—but up to nearly half of LMICs’ populations. In the past 3 decades, child mortality halved to 7 million child deaths per year today. Lifetime morbidity increased to 145 million years lived with disability globally and, in most countries, neonatal disorders and congenital birth defects make up the first or second highest cause. While this underlines the progress made in combatting and preventing infectious disease, improving maternal health care, and scaling nutritional programs, it also highlights the gross lack of progress made in children’s surgical care. 1 in 100 babies are born with congenital heart defects, children with clubfoot are unable to attend school, and infants with cleft lips are ostracized from communities. Congenital defects make up 10% (in low- and lower-middle-income countries) to 20% (in upper-middle-income countries) of all under-5 deaths. Among 5- to 14-year old children, injuries cause up to 50% of all deaths in LMICs. In a majority of existing cases, the answer is simple: surgery—however, commitment to that solution remains stubbornly elusive, even with global agencies well-positioned to push for change.
Since its inception, UNICEF has been dedicated to improving the lives of children around the world, notably through preventive and (mostly medical) curative health care. And yet, UNICEF rarely mentions “surgery” beyond conflict settings. That’s odd, given the current high burden of children’s surgical disease. Professional societies such as the Global Initiative for Children’s Surgery move the needle towards the inclusion of children’s surgery in child health movements and the global health agenda, but much work remains. Earmarked funding and a lack of political commitment to strengthening surgical systems funnels through to the level of children’s surgical care, knowingly or unknowingly.
GICS is working to make sure LMICs have a voice in the efforts. It recently held its fourth biannual meeting in Johannesburg, South Africa (January 17-18), after previous meetings in the UK, the US, and India. The meeting convened over 250 pediatric surgeons, residents, medical students, nurses, and researchers from over 40 countries. Notably, GICS provided travel funding for nearly 150 participants— from Papua New Guinea to Peru—placing equity and capacity-building above anything else. Topics ranging from clinical research to health systems interventions, the role of civil society to academic capacity, and philanthropy to global health advocacy filled 2 days of engaging discussions and networking. Notably, GICS emphasized its efforts to scale pediatric surgical training programs in sub-Saharan Africa in collaboration with KidsOR and the College of Surgeons of Eastern, Central, and Southern Africa.
GICS and its members’ contributions are pivotal to bringing children’s surgery to the heart of health systems strengthening in LMICs. GICS recently developed the landmark Optimal Resources for Children’s Surgery report, which provides recommendations for governments, policymakers, and funders to build capacity to manage children living with surgical disease at every facility level. As LMICs around the world develop National Surgical, Obstetric, and Anesthesia Plans, they increasingly include children’s surgery in these plans. Nigeria, the sixth country to launch an NSOAP, was the first to do so; Pakistan is following suit—for good reason, as 150 million children live in these 2 countries alone. Both countries have embraced the integration of the Optimal Resources framework within their NSOAPs, paving the way for more countries to follow suit.
Today’s children are 2030’s hope. They are more likely than ever to reach adulthood, but complacency is just around the corner. As more survive brushes with infectious diseases in early childhood, children and adolescents are now subject to the largest proportional morbidity burden in history, putting strain on families, impeding socioeconomic growth, and preventing children from reaching their full potential.
Investments in and commitment to children’s surgery are urgently needed; otherwise, history will judge us harshly.
Dominique Vervoort, MD is an aspiring pediatric cardiac surgeon pursuing a Master in Public Health and Master in Business Administration at the Johns Hopkins Bloomberg School of Public Health and Johns Hopkins Carey Business School. Dominique previously completed the Paul Farmer Global Surgery Fellowship at Harvard Medical School, working on National Surgical, Obstetric, and Anesthesia Planning in Pakistan and West Africa.
Join the tens of thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday enewsletter, and please share the link with friends and colleagues: https://www.globalhealthnow.org/subscribe
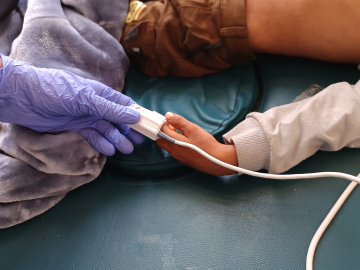
A Syrian doctor checks on a child after a surgery at a hospital in Syria's Idlib province, September 10, 2018. Image: Aaref WATAD/AFP/Getty