What to Watch for in the Coronavirus Outbreak
The new coronavirus that's infected hundreds of people and reached 5 countries has public health officials grappling with the possibility of severe pandemic.
Human-to-human transmission was confirmed on Monday, sharply raising global concerns. The same day, the WHO announced it would convene an emergency committee today to consider whether the outbreak should be declared a Public Health Emergency of International Concern.
While the coronavirus appeared to be simmering since it emerged in December from a seafood market in Wuhan, China, its ability to pop up in multiple countries wasn’t entirely a surprise to researchers at the Center for Health Security at the Johns Hopkins Bloomberg School of Public Health. CHS created a simulation exercise last October called Event 201 that was based on a theoretical coronavirus outbreak (though that one began in South America rather than Asia).
To learn more about the current outbreak and what might happen next, GHN caught up with Crystal R. Watson, DrPH, MPH, a CHS senior scholar.
The coronavirus outbreak has now led to cases in five countries and there’s documented human-to-human transmission. How concerned are you about its potential to become a severe pandemic?
We don’t have enough epidemiologic information to really determine how efficiently this spreads from person to person and how severe the infection is on average for most people. So there’s a lot of unanswered questions right now, but [it’s] highly concerning.
Are there specific signals that you’re looking for, that would make you think, “Oh, no. This is definitely going to get worse.”
If we see significant spread outside of Wuhan and China as a whole, in the next few days, that will be concerning. If we have documented evidence of sustained human-to-human transmission, that would be highly concerning. That’s not what we've had with past major coronavirus outbreaks. [With] SARS and MERS, it was more limited to close contacts, family members, contact with hospital personnel, health care workers. If we start to see more severe infections in people that are otherwise healthy, that would be concerning.
An emergency committee at WHO is meeting today [Wednesday, January 22] to consider a Public Health Emergency of International Concern. What happens then if that does actually occur?
What that does is help to raise awareness internationally about what’s going on. It helps to mobilize additional resources and really get people pulling together to respond to this outbreak internationally.
Does that extend to things like travel restrictions? Is that a possible next step?
The World Health Organization recommends against travel restrictions. The US and other countries may issue travel advisories to make people aware of what’s going on and maybe to recommend that [only] essential travel should go forward. But there are significant economic and societal consequences from seriously restricting travel or closing borders, which is the most extreme response.
One of the things that we’ve already seen are the airport screenings in Asia as well as in the US. How effective are these?
It’s mixed. The evidence that we have from past responses, in particular SARS, but other responses to epidemics as well, is that it’s a huge amount of effort to do fever screenings at airports [but] fairly limited public health benefit. It’s understandable that people want to do something to screen passengers, but we have to think as a public health community carefully about what the actual public health benefit of that is versus the resources that it requires to implement, especially as this grows.
Why did the Center pick a coronavirus for the Event 201 simulation last fall?
We picked a coronavirus because we’ve had some experience with coronavirus outbreaks in the past that have been concerning—MERS and SARS in particular. It was a believable scenario. We’ve seen spillover events from animals to humans before with coronaviruses. And it’s a respiratory pathogen. Some of the research we’ve done here to look at what would most likely be the cause of a future pandemic would be a respiratory pathogen.
There have been the predictable comparisons of the response in this outbreak and the 2003 SARS outbreak in China. What’s your take on how China has handled this outbreak so far?
I think there are some really bright spots. It looks like we are finding out about this outbreak fairly early. With SARS, it was 3 months before it became internationally known that there was an outbreak happening. We also had the release very quickly of the genetic sequence of the [current] virus. Transparency is very important in public health. And so the more transparent that China can continue to be with the ongoing outbreak and the epidemiology, that is all to the good.
There’s probably a mixture of we just don’t know what’s going on yet and maybe some delays in releasing some information, but we’re not really clear on what those delays are. So we’re anxiously waiting to learn more. Overall, the picture has been fairly positive.
Anything else governments should be doing?
If this gets worse, [the US government] should start thinking about what resources we want to put into response. That starts with the funding picture. In past outbreaks like Ebola and Zika, Congress has passed emergency appropriations to support public health response and also scientific research and development of medical countermeasures like vaccines and drugs. So, we ought to be thinking about whether that is something that we want to start pushing forward if this continues to worsen.
Ed. Note: This interview has been edited for length and clarity.
Join the tens of thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues: https://www.globalhealthnow.org/subscribe
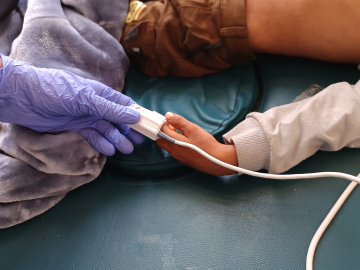
A medical team transfers a patient to Jin Yintan hospital in Wuhan, China on January 17, 2020. Image: Getty