Depression, Pain, Breathing Problems—and That’s After Surviving COVID-19
For Jenessa Thomas, a 44-year-old marathon runner and nutritionist in central Oregon, the first surprise was waking up one morning in mid-March with a rapid heartbeat. The next day, she borrowed a pulse oximeter and got a reading in the high 70s, far below the 95-100 normal reading.
It had to be wrong, she figured. But it wasn’t.
What followed was a positive coronavirus test and solid agony—severe shortness of breath, terrible headaches, body chills, fatigue and pain. “I breathed like I was 25 miles into a marathon—I concentrated on one breath at a time,” she says.
2 weeks after the symptoms started, they disappeared—only to come back the next day. Today she still suffers bouts of crushing fatigue, chest pain, and high blood pressure. “I don’t know where it’s going,” she says.
How many people suffer long-term effects, and for how long, is COVID-19’s biggest mystery. Search the word “sequelae” (after-effects of a disease) in WHO’s global coronavirus literature database, and you get more than 800 results connecting COVID-19 to all sorts of problems—everything from anosmia to gambling, depression, and pneumonia. But no epidemiological study following thousands of people over time has yet revealed the long-term impacts on health and their duration.
The closest thing is the COVID Symptom Study app designed by the Massachusetts General Hospital, King’s College London, and the Harvard T.H. Chan School of Public Health. Brits and Americans who know or suspect they have COVID-19 use the app to regularly report their symptoms. Andrew Chan, MD, MPH, one of the developers of the app, says of the 3.8 million app users, some 300,000 of them are reporting chronic long-term symptoms. But he’s not ready yet to discuss trends or predictors.
Months of clinical experience have shed light on COVID-19’s clinical course, but there is still lots of uncertainty left, said physician Dhruv Khullar, MD, MPP, of New York-Presbyterian Hospital. “I can understand why people are frustrated at not knowing exactly what to expect going forward. In that sense I think clinicians also feel the frustration,” he says.
Khullar, who wrote a piece for The New Yorker on post-COVID-19 care, says older age and other medical conditions can predict a rougher course. “The fair answer is to tell [patients] we don’t know,” he says. “The idea that uncertainty pervades medicine is not new at all, [but] the uncertainty has a really big emotional and mental burden.”
Several Covid-19 experts suggest patients ask their health care providers specifically about what to do as the disease resolves. But solid advice about how to speed recovery and cut the risk of long-term sequelae can be hard to come by, in no small part because there’s not much research to guide it.
Jenessa, for one, would love to start training for a marathon, but if she exerts herself one day she feels awful the next. Several respiratory specialists issued recommendations for athletes in The Lancet in April that called for caution. Cardiologists publishing in JAMA Cardiology note that acute cardiac injury and myocarditis is far more common in people hospitalized with COVID-19 than with other viral infections, and its frequency in infected people outside the hospital is unclear. The cardiologists recommend rest and monitoring for people who are virus-positive but asymptomatic, and they also recommend testing for athletes with moderate to severe symptoms before going back into training.
As for mental health, there’s one group of COVID-19 patients where clinicians fully expect to see long-term problems—people who’ve been in intensive care units. E. Wesley Ely, a pulmonary and critical care specialist at Vanderbilt University, says being in the ICU alone is enough to hurt the brain. Patients may suffer from lack of oxygen, small blood clots in capillaries, toxic effects of sedatives, and the death of neurons.
“ICU survivors have a 50% rate of dementia, a third have depression, and 15 percent have PTSD,” he says, in a time frame of weeks to months after initial recovery. “We think COVID survivors will have at least that and probably more.”
Again, solid numbers have yet to come in, but Ely at least is confident of the brain damage trend. “People on ventilators are going to experience it worse,” he says. “And the younger you are and the less severe your illness is, the less likely you are to have a problem.”
His hospital and others around the country are setting up clinics for COVID-19 ICU survivors to help them with cognitive functioning and mental health therapy. “Many hospitals don’t have these programs in place, so these people are going to suffer a great deal on the back end of their COVID,” he says. “As if COVID wasn’t bad enough.”
Several hospitals, including Khullar’s, have started clinics for any COVID-19 patient so they can access mental health care, physical rehabilitation and other health services.
Jenessa says the anxiety of the unknown is haunting her. “I wish I could find a local survivors’ group where we couple provide a little emotional support and compare symptoms and compare what’s happening,” she says.
“It’s all so strange.”
For the latest, most reliable COVID-19 insights from some of the world’s most respected global health experts, see Global Health NOW’s COVID-19 Expert Reality Check.
Join the tens of thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues: https://www.globalhealthnow.org/subscribe
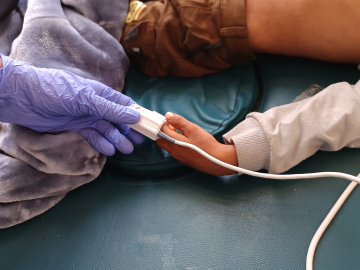
A nurse monitors a COVID-19 patient in the ICU of Regional Medical Center in San Jose, California on May 21, 2020. Image: Justin Sullivan/Getty Images)