How Can Hospitals Handle the Surge in COVID-19 Cases?
Hospitals facing a possible need for 5X to 10X the number of beds they have. Doctors and nurses resorting to bandanas because they lack masks. Refrigerated trucks outside hospitals holding the dead.
It’s been more than a century since the US health care system has faced anything like the COVID-19 pandemic.
The challenges confronting hospitals, doctors, and nurses will likely mount in the coming weeks, says Vivek Murthy, former US Surgeon General and current Distinguished Policy Scholar in Health Policy and Management at the Johns Hopkins Bloomberg School of Public Health. Even so, Murthy finds encouraging signs of resilience.
What are you hearing from physicians and others working in hospitals around the US?
It's mixed. There's a tremendous sense of mission and commitment that people are feeling. They know that they are the front lines. There's a sense of comradery and solidarity. They know this is their moment to step up and serve.
At the same time. I'm also hearing a lot of anxiety and fear as a few people realize that we are not as prepared as a country as we should be. And that our health care systems are not as supported as they need to be to respond to the large influx of patients.
What else are they saying?
They're telling me that in many cases the hospital has run out of masks, so they're bringing in scarves and bandanas from home, even though they know that that's not as effective in protecting them. The part that breaks my heart is that we are sending our doctors and nurses and health care workers into a war without the armor and protection that they need. And we would never think that that was okay to do with our military.
[Some] people are saying that their hospitals are starting to run low on gloves and on gowns. I'm hearing from doctors who are trying to manipulate ventilators to be able to serve more than one patient at the same time because they just need to find a way to meet the capacity needs that are going to come in the next few weeks.
With doctors and nurses relying on bandanas and scarves, how are they going to be able to stay healthy in situations where they're exposed every day?
That is the big worry. We've already started to see health care workers get sick around the world. Italy has had over 3,000 health care workers infected with COVID-19. We're starting to see more doctors and nurses fall ill here in the United States. We also are going to end up losing them at a time when we need them the most. It's a critical issue. We've got to get them to personal protective equipment that they need.
Obviously major hospitals have had emergency plans set for severe flu epidemics, but how useful are those in the absence of these critical supplies?
I think it's safe to say that very few health care systems were prepared for this kind of onslaught. Because this is just outside the scope of what anybody has seen in about a century.
Many hospitals in some of the hardest hit cities are projecting that their needs for intensive care unit beds and overall beds will be between 5X and 10X their total current capacity. I'm not talking about needing a couple hundred more beds, I'm talking about needing thousands of more beds.
What about hospitals that haven't yet seen the surge of patients that likely will be coming—what should they be doing right now?
Number 1, they should assume that the surge very well may come. There's a possibility they may be spared, but we all have to prepare as if it's coming. Number 2, they have to think about 3 critical areas where they may fall short. One is on beds, the second is materials and equipment—that includes ventilators and personal protective equipment like masks, gowns and gloves. And the third area is in the health care workforce. As people start to get sick, as they are under suspicion for infection and get pulled out and quarantined, how are we going to replace those people and extend our health care worker capacity?
Replacing the health care workers—how can that be done?
There are encouraging signs out there, which is exciting and speaks to the power and resilience of the human spirit. We've already seen in New York is that thousands of retired doctors are now stepping up to come back into the workforce to say, "Hey, we are here to help."
We're seeing factories around the country are voluntarily switching their production facilities to make masks and gowns and gloves. We have distilleries that are switching to making hand sanitizer. Recognizing that the only way we will get through this pandemic is if we stick together, if we step up together and ask what we can do to ultimately serve. We have to ask, "What can we do in this moment of great need?"
Ed. Note: This interview has been edited for length and clarity.
View GHN’s latest coronavirus news.
For the latest, most reliable COVID-19 insights from some of the world’s most respected global health experts, see Global Health NOW’s COVID-19 Expert Reality Check.
Join the tens of thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues: https://www.globalhealthnow.org/subscribe
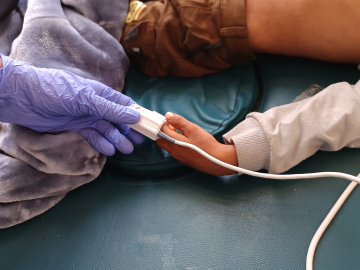
Doctors test hospital staff in a tent outside St. Barnabas hospital in in New York City on March 24, 2020. Photo: Misha Friedman/Getty Images