Health Care Facilities Are Everyone’s Frontline
COVID-19’s multiple frontlines now include at least 46 countries across the African continent. Many, including Ethiopia, have frontline health care facilities battling without one of the most critical tools: adequate water and sanitation.
In an email as truth-telling as it is disturbing, my colleague and friend, Shimeta, ordered his employees to work from home by the time his country was reporting 19 cases (the count is now ~44): “Medical facilities and structures are very weak to handle such pandemic diseases. In Africa and especially in Ethiopia, the death toll will be unheard of up until now. One of the small advantages is that if this outbreak had started in Africa, the world would have heard of it very late, as was the case with the Rwandan genocide and Ebola in DRC.”
Ethiopia’s rural southwest was once my home. My dad moved his young family there from New Mexico and when he volunteered in the local health clinic, I would tag along. When I was 8-years-old, I remember a woman came in, in extraordinary pain. She’d been in labor for days. Her baby was dead and though my father tried, he could not save her life.
I became a doctor. In my work with Ethiopian women suffering from childbirth injuries, things have not improved nearly as much as they should. Women still die in childbirth by the hundreds of thousands globally and health care systems remain dilapidated. In 2016, my organization surveyed 14 rural health posts in Ethiopia. Not one had access to consistent water and sanitation—undercutting everything from the ability to prevent maternal and neonatal injury and death, to the spread of diseases. This fundamental global health problem is solvable and now more urgent than ever with COVID19 spreading across low- and middle-income countries.
Drought can be an issue, but missing infrastructure and broken pipes, pumps, faucets and wells are a massive problem. There are different reasons for poor maintenance—lack of funds, training, prioritization, coordination—but the result is always the same: unsafe, undignified health care. I’ve seen women deliver side-by-side in filthy rooms with little water and blood splattered everywhere in a dilapidated regional hospital that serves 1.5 million people. Mothers tell me they are afraid to deliver in such conditions, but they are also afraid to die in labor at home.
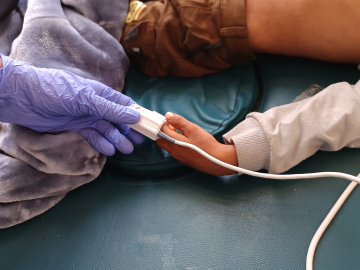
If we think these facilities will be effective against COVID19, consider that health professionals, assistants and cleaners in some areas struggle to wash their hands, let alone much else. Pit latrines overflow in the rainy season spilling patient sewage onto facility compounds; open defecation is common; trash and biohazards are thrown into open, unfenced pits. It’s not just Ethiopia; these conditions are a common sight inside hospitals and clinics in many LMICs. The first UN global baseline report, released in 2019, found that 49% of facilities in sub-Saharan Africa lack basic water services and 64% of health care facilities in eastern and southeastern Asia lack basic hygiene services. 2 billion people must rely on facilities that lack basic water services and 1.5 billion on facilities without sanitation.
Emergency measures to contain COVID19 and prevent resurgence must include global access to Water/Sanitation/Hygiene, WASH. Then health and development leaders, public and private, must make WASH permanent and sustainable. Like other core global health solutions, WASH requires ongoing commitments to funding, training, maintenance and far better coordination.
As leaders focus on vaccines that are months, if not years away, I fear we will continue to overlook the fundamentals of infection prevention and control inside the very places where sick people gather in numbers. Many will die, and we will remain unprepared for the next health crisis. There is simply nothing more effective and nothing more basic to infection prevention and control than WASH. Right now, with a pandemic out of control, what happens in health care facilities is everyone’s frontline.
Margaret “Migs” Muldrow, MD received her medical degree from the Johns Hopkins University School of Medicine and was the Johns Hopkins Centennial Scholar for her humanitarianism in medicine. She is the founder & board chair of the Village Health Partnership based in Denver, Colorado.
Join the tens of thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday enewsletter, and please share the link with friends and colleagues: https://www.globalhealthnow.org/subscribe
This labor and delivery room has no water. CREDIT: Haik Kocharian