We Need to Move Faster to Introduce New TB Drugs
COVID-19’s lethal invasion in late 2019 has turned the world inside out. Yet, another disease, tuberculosis, has been plaguing humans since the Upper Paleolithic era, some 20,000 years ago. In fact, many infection-prevention precautions promoted for the coronavirus—coughing etiquette, distancing, and hand washing—originated as TB-control measures in Victorian times. The COVID-19 response can draw on more challenges and lessons from TB programs that emphasize investments in research and rapid uptake of new diagnostic, prevention, and treatment tools for universal health coverage.
Today, TB is the world’s top infectious disease killer; it claimed 1.5 million lives in 2018 alone. It is difficult to cure, in part because the bacterium that causes it develops resistance to treatments over time. Yet when scientists develop new and effective drugs, countries are slow to adopt them, sentencing thousands in need to die. While the world’s response to TB has rightly taken into account the multitude of socioeconomic factors that fuel its rampant spread, we will not beat the disease if we don’t come up with a faster way to introduce new treatments—especially those that can treat both drug-resistant and drug-sensitive TB, which are more difficult to diagnose.
For example, in August 2019 the US FDA approved a shorter regimen for extensively drug-resistant TB (XDR-TB) under the access-speeding Limited Population Pathway for Antibacterial and Antifungal Drugs policy. Pretomanid, the main medicine in this regimen, was approved based on a limited phase 2B trial of 109 patients. It had an 89% success rate in treating XDR-TB over 6 months, versus 34% over 18 months for the current frontline treatment. However, despite a clear need for a more effective, shorter XDR-TB treatments, WHO is cautious about recommending its use beyond a limited number of patients until there is more evidence of its safety.
Another example is the disappointingly slow initial uptake of bedaquiline, a medication used to treat multidrug-resistant tuberculosis. The FDA approved bedaquiline in 2012, and WHO published interim guidelines for its use in 2013—yet only a small number of countries rushed to adopt and implement it in the first 2 years. Barriers ranged from weak, slow regulatory environments to prescriber hesitation due to lack of knowledge about the new regimen.
Here are the challenges: clinical trials are limited due to funding and human constraints and do not generate enough hard evidence, which slows down approvals by the US FDA and its international equivalents. Combination regimens—the hallmark of all TB treatments—can only be tested after individual medicines are approved for use. Further, regulations in some countries call for local trials and clearances as well, costing more time and money.
So, what can we do?
Health ministries must create supportive regulatory environments—with policies to electronic data tools to speed the processing of applications; and, they must be able to monitor new treatments for success rates and adverse effects. Take Georgia, a small country that received little attention from pharmaceutical companies. After adopting international regulatory standards, it quickly introduced new TB treatments and ensured patient safety through a web-based safety monitoring and management system for bedaquiline and other medicines. The country is now a leader in expedited introduction of innovative treatment solutions.
Donors should continue to fund health system strengthening activities like supporting policies, health information systems, and skills building to help speed drug registration and distribution. For example, through a USAID-funded project, Management Sciences for Health helped 5 countries, including Georgia, introduce bedaquiline by supporting supply chain strengthening and monitoring systems. Strong pharmaceutical systems are a priceless return on investment when it comes to fighting infectious diseases in general, too: any coronavirus or Ebola or malaria treatment will need the same people, processes and infrastructure in place.
Donors must step up to support drug development because they can help gather and document evidence that can speed up adoption. The FDA approved bedaquiline in 2012, but use loitered until USAID partnered with Johnson & Johnson to donate 30,000 treatments to nearly 100 eligible countries in 2015. Then USAID, UNITAID, the Bill & Melinda Gates Foundation, and other donors developed programs to enroll patients on the novel regimens and to collect evidence of their effectiveness. New WHO guidelines further mainstreamed the regimens, and the Global Drug Facility was able to reduce prices, expediting uptake. Thousands of patients received safer treatments and were cured.
Stakeholders must improve collaboration. We have the vehicles: the Critical Path to TB Drug Regimens initiative brings together leading pharmaceutical companies, public health experts, NGOs, and regulatory authorities to expedite research, testing, and approval of promising new drugs—and is always open to new members and support. The European Accelerator of Tuberculosis Regime is an open platform for academic institutions, nonprofits, and research organizations to work on new regimens. In February, the Gates Foundation launched the Project to Accelerate New Treatments for Tuberculosis. Private organizations and NGOs will aim to create novel “pan-TB” regimens of drugs that have little to no resistance and can more efficiently treat all kinds of TB.
We must apply the same sense of urgency that we have shown to developing tests, treatments and vaccines for COVID-19. There are new drugs in development, and there is reason to be optimistic that our efforts will pay off. By taking concrete steps to introduce these medicines and technologies faster and facilitating their uptake via our systems strengthening work, we will make the fundamental changes that we need to get lifesaving medicines to the people who need them more quickly.
Andre Zagorski is a senior principal technical advisor for Management Sciences for Health, a global health nonprofit, and is on the Access Advisory Board for the TB Alliance.
View GHN’s latest coronavirus news here. For the latest, most reliable COVID-19 insights from some of the world’s most respected global health experts, see Global Health NOW’s COVID-19 Expert Reality Check.
Join the tens of thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues: https://www.globalhealthnow.org/subscribe
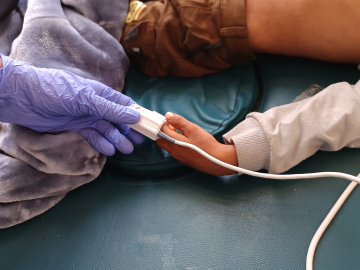
A patient holds a packet of tablets received as part of his treatment at Rutsanana Polyclinic in Glen Norah township, Harare, Zimbabwe, June 24, 2019. Image: Jekesai Njikizana/AFP/Getty