Malaria Services Must be Maintained Amid COVID-19 Pandemic
For the first time in over 100 years, people all over the world are fighting a common public health enemy: COVID-19.
Yet, even as we pour resources into fighting this new pandemic, there is an urgent need to keep up the fight against an age-old enemy: malaria, which continues to cause immense suffering and death among some of the world’s most vulnerable populations. For countries in sub-Saharan Africa, COVID-19’s disruptions to prevention and treatment of malaria could be particularly devastating.
A staggering 769,000 people in the region could die from malaria this year alone if all net campaigns are suspended, and if access to antimalarial medicines is reduced by 75%, according to a new modeling analysis conducted by WHO and partners.
This represents a doubling in the number of malaria deaths compared to 2018 and a return to the mortality levels last seen 20 years ago.
In 2018 alone, the region shouldered more than 90% of the estimated 228 million malaria cases and 405,000 deaths worldwide. Pregnant women and children are particularly hard hit. According to WHO’s latest World Malaria Report, nearly a third of women in 38 sub-Saharan African countries were infected with malaria while pregnant in 2018. As a result, nearly 900,000 children were born with a low birthweight—a major cause of infant mortality. Each year, malaria claims the lives of more than 270,000 young children in the region.
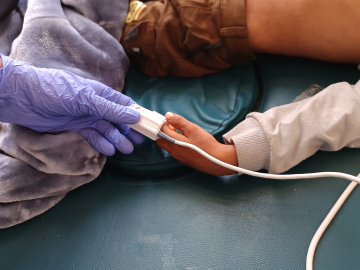
Since 2000, countries have made immense progress in the fight against malaria and have more tools in their arsenal than ever before: nets, preventive therapies for young children and pregnant women, rapid diagnostic testing, and effective antimalarial medicines, among others. The global scale-up of these tools has helped reduce malaria death rates more than 60% over the last 2 decades.
This time last year, under very different circumstances, spirits were high as we celebrated the culmination of 30 years of research and investments through the introduction of the world’s first malaria vaccine in Ghana, Kenya and Malawi. The RTS,S vaccine is a new tool that reduces malaria in children and can ease the strain the illness places on health systems, including lowering hospital admissions and the need for blood transfusions. Over the past year, an estimated 275,000 children have received their first dose of the malaria vaccine across the 3 countries participating in the pilot program.
We cannot afford to lose that momentum. This means maintaining and boosting access to the tools we have at hand while also investing in the research and development of new ones that will be needed to fight—and eventually eradicate—this age-old disease. To support countries in sub-Saharan Africa, which have a critical window of opportunity to save lives before the pandemic spreads widely in the region, WHO and partners have published practical guidance on how to maintain core malaria services in ways that ensure a safe environment for health workers and communities.
A stall in action now will bring unnecessary suffering and loss of life, and place additional—yet avoidable—stress on overburdened health providers, facilities and resources.
We should feel emboldened and inspired by the unprecedented levels of collaboration in the fight against public health’s new enemy, COVID-19, and apply the same to the enemy we know all too well.
Pedro Alonso, MD, PhD, is director of the WHO Global Malaria Programme in Geneva.
For the latest, most reliable COVID-19 insights from some of the world’s most respected global health experts, see Global Health NOW’s COVID-19 Expert Reality Check.
Join the tens of thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues: https://www.globalhealthnow.org/subscribe
WHO/F. Kokoroko